Stem cells are remarkable and versatile cells that hold immense potential for regenerative medicine and scientific research. These unique cells possess the remarkable ability to differentiate into various specialized cell types and self-renew, making them crucial for the development, growth, and repair of tissues and organs within the human body. Stem cell research has opened up new avenues of understanding the fundamental mechanisms of life and has the potential to revolutionize medical treatments by offering novel therapies for previously untreatable diseases and injuries. This app will explore the different types of stem cells, their sources, and their remarkable potential in regenerative medicine, mechanisms of action, and their therapeutic applications in medical and veterinary sciences. We also describe here as well as the ethical considerations surrounding their use.
One of the significant applications of stem cells in medical science is regenerative medicine. Stem cells have the remarkable capacity to repair and regenerate damaged tissues and organs. They can be used to replace or restore malfunctioning cells, such as in the case of degenerative diseases like Parkinson's or Alzheimer's. Stem cell-based therapies have shown promising results in treating conditions such as spinal cord injuries, heart diseases, and diabetes. Furthermore, stem cells play a crucial role in disease modeling and drug discovery. By generating induced pluripotent stem cells (iPSCs) from patients with specific diseases, scientists can create models that mimic the diseased tissues and study their characteristics. This approach allows for a deeper understanding of disease mechanisms, the identification of novel drug targets, and the development of personalized treatment strategies.
A significant application of stem cells in veterinary medicine includes orthopedic injuries and musculoskeletal disorders. Stem cell therapy can aid in the regeneration of damaged cartilage, tendons, ligaments, and bone, offering a non-invasive and effective treatment option for conditions such as osteoarthritis, ligament tears, and fractures. By harnessing the regenerative potential of stem cells, veterinarians can enhance the healing process and improve the overall quality of life for animals suffering from these conditions.
Furthermore, stem cell therapy has been explored in the field of veterinary dermatology. It can aid in the treatment of chronic wounds, burns, and skin disorders by promoting tissue regeneration and reducing inflammation. Recently, stromal vascular fractions (SVFs) obtained from animal adipose tissue have emerged as a valuable and abundant source of mesenchymal stem cells, offering promising potential in the field of wound repair.
In summary, stem cells are versatile cells capable of differentiating into various cell types and self-renewal. In medical and veterinary sciences, stem cells have therapeutic applications. In medicine, they hold promise for regenerative medicine, treating conditions like orthopedic injuries, cardiac diseases, neurodegenerative disorders, and autoimmune conditions. Stem cells aid in tissue repair, restoring function, and improving quality of life. In veterinary science, stem cells are used to treat musculoskeletal injuries, degenerative diseases, skin disorders, and ocular conditions in animals. The application of stem cells offers innovative treatments and improved outcomes. Ongoing research continues to explore their full potential, paving the way for personalized therapies and advancements in regenerative medicine in both human and animal healthcare.
Stem cells are remarkable cells characterized by their unique ability to self-renew and differentiate into various specialized cell types. Unlike mature or terminally differentiated cells, which have limited or no capacity for differentiation, stem cells serve as the building blocks for all other cell types in the body. They differ from mature cells in three key aspects:
- They can divide and renew themselves indefinitely.
- They are unspecialized cells, meaning they do not have specific and specialized cellular functions.
- They divide and produce terminally differentiated cells.
Stem cells can be categorized on the basis of the following:
- A) Based on the source
- B) Based on potency
Embryonic stem cells (ESCs): ESCs are derived from the inner cell mass of the early-stage embryos. They possess two distinctive features: pluripotency and self-renewal. Pluripotency refers to their ability to differentiate into any cell type of the body, giving rise to tissues and organs. ESCs can proliferate indefinitely through self-renewal, maintaining an undifferentiated state. These cells offer immense potential for regenerative medicine and research, as they can be directed to differentiate into specific cell types for therapeutic purposes. However, ethical considerations and challenges associated with immune rejection limit their clinical application, emphasizing the need for alternative sources of stem cells. Naive and primed embryonic stem cells (ESCs) represent distinct states of pluripotency in the developmental journey of these cells.
Naive ESCs are derived from preimplantation embryos and are considered to be in an earlier, less differentiated state. They exhibit characteristics such as unrestricted differentiation potential and a higher capacity for self-renewal. Naive ESCs closely resemble the inner cell mass of the blastocyst and have the ability to contribute to both embryonic and extraembryonic tissues. They are considered to be in a ground state of pluripotency.
On the other hand, primed ESCs are derived from post-implantation embryos and have undergone some level of differentiation. They are more lineage-restricted and have a reduced capacity for self-renewal compared to naive ESCs. Primed ESCs are already committed to specific cell lineages and are more limited in their potential to give rise to various tissue types.
Adult stem cells (ASCs) : Adult stem cells or tissue-specific stem cells, also known as somatic stem cells, are a specialized type of stem cell that exists in various tissues and organs throughout the body. Unlike embryonic stem cells, tissue-specific stem cells are more limited in their differentiation potential, as they can typically give rise to cell types within their respective tissue of origin. ASCs play a crucial role in maintaining tissue homeostasis, regeneration, and repair. They serve as a reservoir of cells that can replenish damaged or lost cells due to injury, disease, or normal cellular turnover. Tissue-specific stem cells are found in organs such as the bone marrow, skin, brain, liver, skeletal muscle, and many others.
Each tissue-specific stem cell population exhibits unique characteristics and functions. For example, hematopoietic stem cells in the bone marrow give rise to various blood cell types, while neural stem cells in the brain contribute to the generation of neurons and glial cells. These cells possess the ability to self-renew and differentiate into specialized cell types, making them essential for tissue maintenance and repair.
Understanding tissue-specific stem cells and their behavior holds great potential for regenerative medicine, as harnessing their regenerative capacity may lead to the development of targeted therapies for various diseases and injuries.
Induced pluripotent stem cells (iPSCs): Induced pluripotent stem cells are a type of pluripotent stem cell that was first generated by Shinya Yamanaka and Kazutoshi Takahashi in 2006 through the introduction of four specific genes: Myc, Oct3/4, Sox2, and Klf4, collectively known as Yamanaka factors. These artificially reprogrammed cells exhibit similar properties to embryonic stem cells (ESCs) in terms of self-renewal and the ability to differentiate into various cell types. iPSCs have gained significant attention due to their potential to address ethical and religious concerns associated with the use of ESCs.. The study of iPSCs offers a promising avenue for understanding disease etiology and has diverse applications, including disease modeling, drug screening, regenerative medicine, and personalized cell therapies. iPSCs offer a valuable tool for understanding disease mechanisms, developing new treatments, and providing patient-specific cell sources for transplantation and tissue regeneration.
Cancer stem cells (CSCs) These are the subpopulation of tumor cells that drive tumor initiation and propagation. At the time of tumor initiation, CSCs can originate either from differentiated cells or tissue-specific stem cells.
Totipotent: This precursor cell type can develop into all subsequent cell types throughout the development of an organism. It applies to single-cell zygotes and their descendant cells from the earliest embryonic divisions. Totipotent cells can produce both embryonic and extraembryonic tissues.
Pluripotent: The stem cell obtained from the blastocyst stage of the embryo has the potential to differentiate into almost every cell type of body, excluding extraembryonic tissues.
Multipotent: The stem cells can develop into cells of specific tissue/organs. For example, a hematopoietic stem cell can develop only into various blood cell types.
Oligopotent: The stem cells that can only develop into a smaller subset of the cell types that compose a more complex organ or tissue.
Bipotent: The stem cells can give rise to two different cell types.
Unipotent: The stem cells that can develop into only one type of cell but possess the potential for self-renewal hence being considered a stem cell.
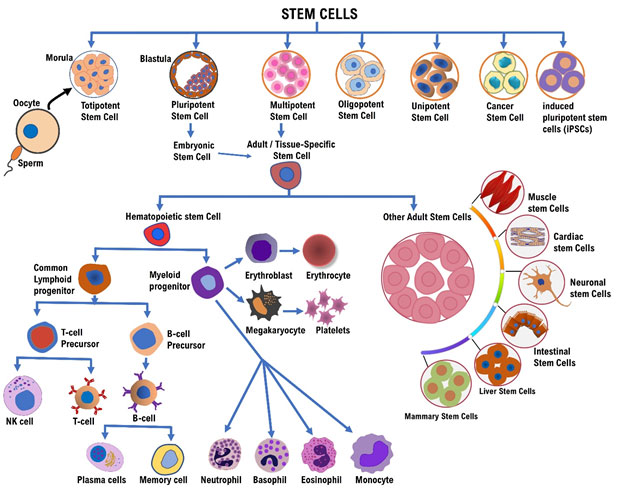
Types of stem cells (Photo: Illustration of Dr. D. Pathak).
The identification of stem cells involves the use of specific markers and techniques to distinguish them from other cell types. Here is a general description of the common methods used for stem cell identification:
Surface Marker Analysis: Stem cells often express unique proteins on their cell surface. Antibodies that target these proteins can be used in techniques like flow cytometry (Fluorescence-Activated Cell Sorting; FACS) or immunocytochemistry to identify and isolate stem cells based on their surface marker expression.
Gene Expression Analysis: Stem cells exhibit characteristic patterns of gene expression. Methods such as reverse transcription-polymerase chain reaction (RT-PCR) or gene microarrays can be employed to detect the expression of specific genes associated with stem cell properties.
Functional Assays: Stem cells possess functional characteristics, such as the ability to self-renew and differentiate into multiple cell types. Functional assays, including clonogenic assays and differentiation assays, can assess the capacity of cells to form colonies or generate specialized cell lineages, respectively.
In vivo, Assays: Transplantation or engraftment of cells into animal models can be used to evaluate the regenerative potential of stem cells. ESCs form embroid bodies when transplanted or injected into immunocompromized mice. The ability to repopulate and differentiate into functional tissues confirms their stem cell identity.
These methods, often used in combination, aid in the identification, characterization, and isolation of stem cells from various tissues and sources.
In the mid 20th century, researchers learned that bone marrow has cells that can develop into every type of blood cell. However, explicitly identifying these hematopoietic stem cells from progenies of stem cells (progenitor cells) remains an unsolved problem in stem cell biology. An array of phenotypically similar but immuno-phenotypically different cells poses difficulty in distinguishing stem cells from progenitor cells and progenitor cells from the early committed progenitor cells. Because of the lack of ASC-specific biomarkers, immuno-phenotypic identification, detection, isolation, and quantification of ‘true’ ASCs remains a significant challenge.
Methods of detection of ASCs are
- *Cell surface markers –CD34+ population of cells containing hematopoietic stem cells (HSCs) or using multiple cell surface markers like Lin–CD34+CD38–CD90+CD45RA– and CD49f+ cells are the ‘true’ population of human HSCs.
- *Morphology of cells – A large nuclear-to-cytoplasmic ratio is the hallmark feature of stem cells compared to a small nuclear-to-cytoplasmic ratio of differentiated cells.
- *Immunohistochemistry(IHC) – based on the expression of protein markers on either cell surface, like CD34, or nuclear, like OCT4.
- *In vitro culture- sphere formation ability – based on the ability of stem cells to grow in non-adherent and 3D conditions, provides a functional assay to estimate the number of the stem cell population.
- Label retention studies- Label retention studies are a valuable approach for identifying and characterizing stem cells within a tissue or population of cells. These studies involve the incorporation of a labeled marker or tracer into cells or tissues, which is retained by cells with specific properties, such as stem cells, over time. One common method for label retention studies is to use a stable isotope label, such as BrdU (bromodeoxyuridine). BrdU is incorporated into the DNA of dividing stem cells. Slow division rates of stem cells allow them to retain the labeled BrdU over an extended period, while more rapidly dividing cells like progenitor cells lose the BrdU label during successive divisions.
- *Colony forming unit assays – only for hematopoietic and endothelial stem cells. The spleen colony unit (CFU-S) assay is a classic in vivo technique used to assess the self-renewal and multipotency of hematopoietic stem cells (HSCs). It involves the transplantation of bone marrow cells into irradiated recipient mice and the subsequent examination of the formed colonies in the spleen.
- Severe combined immunodeficiency (SCID) mouse repopulating cell assay – only for hematopoietic stem cells. This assay is an experimental method used to assess the repopulating capacity and functional properties of human hematopoietic stem cells (HSCs). It involves the transplantation of human cells into immunodeficient SCID mice and subsequent evaluation of their ability to reconstitute the mouse hematopoietic system.
- Kinetic stem cell-based counting- Kinetic stem cell (KSC) counting refers to a method used to estimate the number of viable stem cells in a sample based on their growth and proliferation characteristics over a defined period of time. The KCS approach takes advantage of the unique ability of stem cells to undergo self-renewal and form colonies when cultured in appropriate conditions. This is a technique of precisely counting ASCs based on computationally predicted models to characterize in vitro behaviors of stem cells, namely long-term replication, apoptosis, differentiation, and cell proliferation (Sherley et al., 2022).
* Does not distinguish stem cells from committed progenitor cells
- Differentiation of stem cells to replace damaged cells
- The paracrine activity of stem cell secreted factors called secretome that promotes healing and tissue repair
- Immunomodulation
- Stem cell-mediated transfer of organelles or molecules through tunneling nanotubes (TNT).
- Cell replacement- Fusion of stem cells with differentiated cells to rescue damaged cells
- Tissue protection and anti-apoptosis: Apoptotic bodies of stem cells engulfed by the macrophage to induce cytokine production and healing effects (He et al., 2021)
- Tissue regeneration – helps in growth, repair of damaged tissue, and regeneration to restore the normal function of the tissue.
- Transplantation medicine – transplantation of diseased or cancerous bone marrow with healthy donor-derived bone marrow restores the immune system and blood-related disease.
- Neurological disorders – regeneration of damaged nerve cells and restoration of functionality
- Treatment of immune deficiency diseases – allogeneic transplantation of blood-forming stem cells helps in replacing immune deficiency diseases.
- Treatment of blood anemia diseases—similar to the result obtained from bone-marrow transplantation of healthy bone marrow to anemic patients cures the blood-related disease.
- Wound healing – Stem cell-assisted wound healing therapy is one of the most extensively studied areas. Presently, the strategy of wound healing based on the combinatorial use of stem cells and skin tissue engineering is in use.
- Cancer treatment – chemotherapy and radiation therapies are being used to kill cancer cells. On the one hand, chemotherapy is a systematic treatment, while on the other hand, radiation therapy is often applied to treat localized tumors. Stem cell therapy directly replaces damaged cells and indirectly helps in the ability of the body to produce stem cells after chemo- or radiation therapy.
- Creation of transgenic animals by gene and genome editing – Gene trapping in embryonic stem cells (ESCs) is one of the powerful techniques to create a mutation in transgenic animals. DNA microinjection of ESCs is another method to create transgenic animals.
- Production of chimera – Combining a preimplantation embryo with a genetically similar but modified embryo in vitro and transferring them into a foster mother creates chimera.
- Organ development research – in vitro development of organogenesis utilizes pluripotent stem cells. For example, intestinal, liver, and islets organoids have been developed using ESCs. These tissue organoids can rescue plasma levels of hormones (like thyroid in thyroid mice) post-implantation.
- Plastic surgery research – Stem cells are being used to reverse atopic and photo-damaged cells to rejuvenate skin. Adipose tissue-derived stem cells and iPSCs are being used to form an acellular adipose matrix (AAM) after induction. AAM acts as a scaffold for tissue engineering.
- Gene therapy – The application of genetically corrected stem cells and transplanting them back to individuals can be a new therapeutic approach, alternatively called stem cell gene therapy, to correct genetic diseases caused by gene deletion.
- Assisted reproductive medicine – Stem cells have shown promise in various aspects of assisted reproductive medicine, offering potential benefits for both infertility treatment and reproductive research. Here are some notable uses of stem cells in this field:
-
- Female infertility treatment
- Male fertility treatment
- Gamete and embryo development
- Reproductive tisssue regneration
- Reproductive research and drug development
In veterinary patients, stem cells, especially mesenchymal stem cells (MSCs), are used for treating horse, dog ligaments, cartilage, and joint injuries. Bone marrow or adipose tissue-derived MSCs are used for the treatment of various following diseases:
- Wound healing – in dogs, one of the most extensively studied applications of stem cells
- Tendonitis- inflammation of the tendon – in horse
- Cartilage injury - in dogs and horse
- Renal conditions – in old and aged cats, improved outcomes were noticed in nephritis, fibrosis, and tubular atopy.
- Musculoskeletal disease – lameness in the horse, osteoarthritis in canines
- Digestive tract diseases – gastrointestinal inflammation, inflammatory bowel disease in dogs
- Reproductive systems
Testis xenografting – to preserve genetically valuable prepubertal male animals
Spermatogonial stem cell transplantation – to manipulate male germ line
- Eye disease – Keratoconjunctivitis sicca (KCS) – in dogs
- Heart disease – myocardial infarction, dilated cardiomyopathy
- Neuromuscular disorders – treatment of spinal injury using allogeneic and autologous MSCs in dogs
- Mastitis – stem cells have shown promising and hopeful results in treating acute and chronic mastitis of bovine. In addition to the treatment of inflamed udder, the role of stem cells in maintaining mammary health and milk production.
Utility stem cells in treating various diseases with some possible clinical applications in bovines (Figure 2) and canines (Figure 3) have been provided.
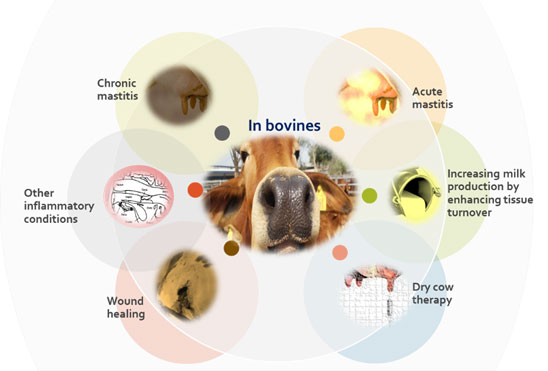
Figure 2: Stem cell applications in bovine medicine can be exploited for treating diseases and increasing milk production.
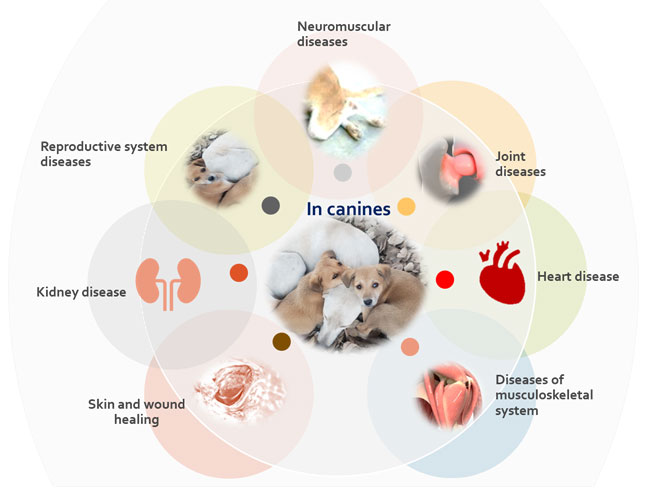
Figure 3: In canines, stem cells are being investigated for suitability in treating many chronic, debilitating, and currently untreatable diseases.
In the medical field, various types of stem cells, namely, embryonic stem cells (ESCs), mesenchymal stem cells (MSCs), bone marrow stem cells (BMSCs), umbilical cord stem cells (UCSC), and induced pluripotent stem cells (iPSCs) are used for therapies and therapeutic development. Associated progenitor cells (PCs) are also used for cell therapy development. MSCs usage in regenerative medicine includes:
- Heart scar repair after an attack - Scientists have found promising results of stem cells in repairing damaged heart muscle. Out of many studies, in a study conducted on 31 patients, stem cells derived from the patients or from healthy volunteers reduced heart muscle scar tissue.
- Liver transplantation - Many animal studies and clinical trials have indicated the efficacy of stem cell transplantation in patients with liver diseases like cirrhosis, liver failure, and hepatic tumors.
- Muscle degeneration – Delivery of muscle satellite cells using hydrogel and stem cell products found to help patients with muscle injuries. Satellite cells are the adult stem cells of muscle tissue that maintain skeletal muscle integrity. Applications of stem cells in treating sarcopenia (age-related skeletal muscle disorders like loss of muscle mass, tonicity and functions) is a realized novel therapeutic approach.
- Ligament regeneration -A number of researchers have worked on animal models to show the healing for partially transected ligaments and histologic re-approximation of bone-tendon interface after using mesenchymal stem cells.
- Cartilage regeneration – Stem Cell-based therapy has been found useful in articular cartilage damage, and the articular regeneration treatment is in Phase 3 trial in 2022.
- Regeneration of joint tissue – Stem cells, when injected into the joint, showed healing of injured tissue of the knee, shoulder, or elbow.
- Alopecia – Treatment for hair loss that focuses on reactivating hair follicle stem cells regenerating and grown new hair. For transplantation of hair follicle stem cells, stem cell-derived conditioned medium and stem cell-derived exosomes have been found useful in treating alopecia.
- Restoration of erectile dysfunction – The clinical study on treating erectile dysfunction (ED) started in 2010, in which an injection of 1.5 million umbilical cord blood stem cells injected in aged persons regained morning erections till six months.
- Bladder deformities – Urinary bladder deformities like decompensation- the inability of bladder smooth muscle cells to properly metabolize extrinsic calcium, causing obstruction and, ultimately, stone formation. Ongoing studies are directed toward reconstructing bladder tissue deformities using mesenchymal stem cells.
- Congestive heart defects (CHD) –CHD constitutes the most prevalent congenital anomalies of the heart. Stem cell delivery, along with the palliative surgery of a defective heart, showed beneficial effects over the surgery alone.
- Neurogenerative disease – Several preclinical studies have suggested the potential benefits of mesenchymal stem cell therapy in treating neurological diseases. Considering the ability of stem cells to secrete neurotrophic factors, immunomodulators, and even organelle donors (like mitochondria), MSCs therapy holds promise for the treatment of Parkinson’s disease.
- Anemia and blood cancer - As indicated before, bone marrow transplantation from a healthy donor ‘rescues’ anemia and blood cancer-related issues.
- Treatment of acquired immunodeficiency syndrome (AIDS) – Treatment of acquired immunodeficiency syndrome (AIDS) was done using anti-HIV hematopoietic stem/progenitor cell (HSPC)-directed gene therapy. Multiple strategies of stem-cell-based gene therapy have been suggested to infer HIV resistance, including anti-HIV gene-modified stem cells. Like genetically engineered stem cells will possibly interrupt key stages of HIV proliferation.
- Orodontal deformities – Various types of tissue-specific stem cells of oral environment like dental follicle stem cells stem cells of the apical papilla, dental pulp stem cells and periodontal ligament stem cells, bone marrow-derived MSCs including oral-derived iPSCs have been shown to improved results in dentistry, during preclinical trials using animal models.
- COVID-19-associated acute respiratory distress syndrome (ARDS) – In recent years, MSCs and lung progenitor cells have been used to treat acute lung damage caused by the COVID-19 virus. Due to the powerful immunomodulatory regulatory roles of MSCs, stem cells have been the spotlight roles in improving lung function, reduction in lung injury, and alleviating lung fibrosis in COVID patients.
- Graft versus host disease (GVHD) – GVHD is a life-threatening complication that occurs due to allogeneic transplantation of hematopoietic stem cells. On the contrary, mesenchymal stem cells are generally safe and have largely been used for the treatment of acute and chronic GVHDs.
- Chronic obstructive pulmonary disease (COPD) – COPD is a chronic and destructive disease of the lung. Because of its anti-inflammatory, immunomodulatory and reparative properties, MSCs therapy may provide a therapeutic option. However, in large multicentric randomized trials, stem cell therapy does not support the restoration of lung function by stem cells.
Umbilical cord blood stem cells (UCSCs): Umbilical cord blood stem cells are a type of stem cell that are collected from the blood present in the umbilical cord and placenta after a baby is born. They are considered a rich source of hematopoietic stem cells (HSCs) and are widely used in medical treatments and research. UCSCs are a rich source of MSCs and other cell types like hematopoietic stem cells (HSCs) and progenitor cells. Umbilical cord blood stem cells have revolutionized the field of transplantation and offer significant potential for therapeutic applications.
UCSCs can be collected and stored in cord blood banks for future use. Cord blood banking allows families to preserve the stem cells for potential medical treatments, either for the baby or for compatible family members. Public cord blood banks are also available for individuals to donate their cord blood for use by others in need.
The ex vivo expansion of UCSCs is useful in many clinical applications, including:
- Treatment of diabetes by replacing pancreatic cells – limited success thus far
- Tendonitis
- Regeneration of hyaline cartilage of the knee
- Treatment of neuroblastoma
- Treatment of Krabbe's disease: Krabbe’s is a rare inherited metabolic disorder and is related to the accumulation of dangerous amounts of lipids in many cells and tissue of the body, finally leading to the killing of brain cells. Hematopoietic stem cells (HSCs)
- HSC therapy for pediatric leukemia treatments
- Clinical trials for autism treatment
Induced pluripotent stem cells (IPSCs): iPSCs are formed by reprogramming somatic cells using various transcription factors. iPSCs have unique self-renewal properties and can differentiate into many types of cell lineage. Hence, iPSCs are a potential replacement for embryonic stem cells (ESC) for treating various diseases. The use of iPSC may overcome several ethical and religious issues related to the use of embryos (ESC) in research and clinical trials. iPSCs provide patient-specific scalable cells of various tissue types for pathophysiological study, cancer study, toxicity assay, and drug screening. Applications of iPSCs in human regenerative diseases are;
- Alloimmune platelet transfusion refractoriness
- Treating lung defects
- Heart valve generation
- Lung and liver disease
- Kidney regeneration
- Brain defects like Alzheimer's
- Pacemaker recovery
- Treatment of blood and immune cells defects
- Regeneration of pancreases
- Vision restoration